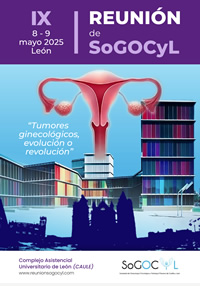
IX Reunión de la Sociedad de Ginecología Oncológica de Castilla y León
Nos complace invitaros a la IX Reunión de la SoGOCyL, que se celebrará en León los días 8 y 9 de mayo de 2025.
VIII Reunión de la Sociedad de Ginecología Oncológica de Castilla y León
Este 2023 nos complace anunciar que la VIII Reunión de la SoGOCyL tendrá lugar los días 16 y 17 de noviembre en Valladolid.
VII Reunión y I Online SoGOCyL 2021
En 2021 la Reunión de la Sociedad de Ginecología Oncológica de Castilla y León se celebrará online los días 2 y 3 de junio.
Jornadas SoGOCyL 2020
La VII Reunión de la Sociedad de Ginecología Oncológica de Castilla y León tendrá lugar los días 7 y 8 de mayo de 2020 en León.
II Reunión de la Sociedad de Ginecología Oncológica y Patología Mamaria de Castilla y León.
Escrito por Administrator Martes, 24 de Enero de 2012 16:49Nos complace anunciar que cada vez está más cerca la II Reunión de la Sociedad de Ginecología Oncológica y Patología Mamaria de Castilla y León.
Estudio Vulcan - Estudio Multicéntrico sobre Cáncer de Vulva
Escrito por Ana Isabel Gomez Calvo Martes, 18 de Octubre de 2011 08:10Queridos amigos y compañeros,
Un año más, nos disponemos a desarrollar un trabajo transversal multicéntrico para mejorar el conocimiento de una patología oncológica concreta, y en el que al igual que años anteriores, nos gustaría que todos participaseis como investigadores. En este caso la patología elegida ha sido el CARCINOMA DE VULVA, con la peculiaridad de que no sólo obtendremos datos a nivel nacional, si no también a nivel europeo, a través de la European Network of Young Gynecologist Oncologists (ENYGO) afiliada a la Sociedad Europea de Ginecología Oncológica (ESGO).
ACTA DE LA 1ª REUNIÓN INFORMATIVA DE LA SoGOCyL
Escrito por SoGOCyL Sábado, 30 de Abril de 2011 10:11ACTA DE LA 1ª REUNIÓN INFORMATIVA DE LA SoGOCyL
León 15 de Abril de 2011. Inicio 20:30 horas
Orden del día:
1. Bienvenida y Agradecimientos
En general a asistentes y ponentes.
En particular a los Dres. Peñalosa y Cabezas por la facilitarnos infraestructura de la SoGICyL para este Evento.
Axillary Dissection vs No Axillary Dissection in Women With Invasive Breast Cancer and Sentinel Node Metastasis
Escrito por SoGOCyL Miércoles, 27 de Abril de 2011 22:16Axillary Dissection vs No Axillary Dissection in Women With Invasive Breast Cancer and Sentinel Node Metastasis
A Randomized Clinical Trial
Armando E. Giuliano, MD, Kelly K. Hunt, MD, Karla V. Ballman, PhD, Peter D. Beitsch, MD, Pat W. Whitworth, MD, Peter W. Blumencranz, MD, A. Marilyn Leitch, MD, Sukamal Saha, MD, Linda M. McCall, MS, Monica Morrow, MD.JAMA, February 9, 2011—Vol 305, No. 6
Context Sentinel lymph node dissection (SLND) accurately identifies nodal metas-tasis of early breast cancer, but it is not clear whether further nodal dissection affects survival.
Objective To determine the effects of complete axillary lymph node dissection (ALND) on survival of patients with sentinel lymph node (SLN) metastasis of breast cancer.